Introduction
Studies have shown that HBOT is the advanced strategy for treating diabetes-related complications, but hyperbaric oxygen therapy is not a routine treatment for diabetes-related complications.
It plays a key supporting role in only one specific, extremely troublesome complication: diabetic foot ulcers (Diabetic Foot Ulcer, DFU).
Specifically, in our clinical treatment of diabetic complications, hyperbaric oxygen therapy is used primarily for chronic, refractory wounds that have not healed by standard care, especially in patients with evidence of limb ischemia and local tissue hypoxia.
Why would someone get this disease?
Neuropathy: Sensory nerves are damaged, causing the patient to lose consciousness to pain, pressure, and temperature, often without noticing minor injuries.
Vascular lesions: long-term high blood sugar caused by microvascular and macrovascular damage, resulting in a serious shortage of blood supply to the foot. The oxygen and nutrient supply of the wound site is extremely scarce, making the tissue in a hypoxic and hypoxic state, and the cells in the wound area cannot proliferate and repair.
Immune dysfunction and infection: poor blood supply and impaired immune cell function make any small wound prone to secondary serious infection, further aggravating local tissue hypoxia and necrosis. And the hyperglycemic environment itself weakens the function of immune cells, making it easier for infections to occur and spread.
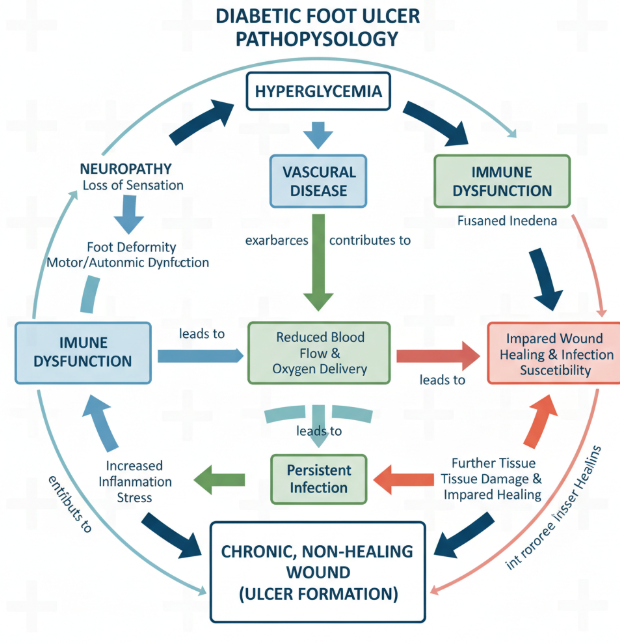
These three mechanisms interact to form a vicious circle, so that the wound has been in a state of hypoxia, chronic inflammation, can not be closed.
How does hyperbaric oxygen treat the condition
Therapeutic Principle of Hyperbaric Oxygen
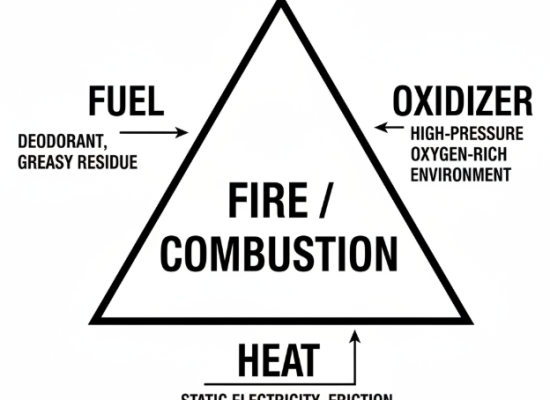
At the heart of HBOT is the use of high-pressure environments to achieve plasma supersaturation oxygenation.
Inhaling 100 percent pure oxygen at two or 3 atmospheres of absolute pressure (ATA), the partial pressure of oxygen in the blood can soar from about 100 mmHg in normal arterial blood to an astonishing 1000-2000 mmHg. These high pressures cause large amounts of oxygen to dissolve directly in the plasma.
Due to long-term high blood sugar, the microcirculation of diabetic patients is often blocked, and the oxygen-carrying red blood cells cannot pass through these narrow blood vessels to reach the deep wound.
However, the oxygen dissolved in the plasma, which does not rely on red blood cells, can penetrate into the deepest part of the ischemic tissue in the form of fluid, effectively bypassing those channels blocked by microvascular lesions, so that the diseased part gets sufficient oxygen supply.

How Does Hyperbaric Oxygen Act on The Condition
Induction of angiogenesis and long-term repair:
Periodic high pressure, high oxygen environment can stimulate the growth and differentiation of endothelial cells, directly promote the formation of new blood vessels, that is, in the ischemic area to build new oxygen and nutrient channels.
Directly support cellular function and collagen synthesis:
Key to wound healing, such as fibroblast proliferation, hydroxylation and deposition of new collagen, require oxygen as a coenzyme or substrate. The high-oxygen environment provided by hyperbaric oxygen provides the necessary raw materials for these cell activities, so that they can start to work.
Enhance white blood cell function and bactericidal ability:
In diabetic foot infections, the phagocytic and bactericidal functions of leukocytes are impaired, in part because of local hypoxia. A hyperoxic environment can greatly enhance the ability of these immune cells to carry out “respiratory bursts. Respiratory burst is a key process by which white blood cells produce reactive oxygen molecules such as superoxide and hydrogen peroxide to kill bacteria. At the same time, hyperoxia has a direct toxic effect on anaerobes (a class of bacteria common in DFU infections).
Reduce edema and inflammatory reactions:
Hyperbaric oxygen causes moderate local vasoconstriction, which helps to reduce inflammatory edema around the wound. By reducing edema, HBOT indirectly improves the perfusion state of the tissue, creating a positive cycle.
Clinical Guidelines
- Strict Screening for Indications: Clinical guidelines require chronic refractory ulcers of Wagner grade 3 or higher that have not significantly healed after receiving standard care for at least 30 days including debridement, decompression, and infection control.
- Treatment parameters: A typical treatment regimen is usually set at 2.0 to 2.5 ATA, each lasting 90 to 120 minutes, and a complete course of treatment may take 20 to 40 times.
HBOT Limitations and Contraindications

Limitations:
- Cost and accessibility: HBOT equipment is expensive, treatment costs are high, and it usually requires a once-a-day treatment cycle lasting several weeks, which is time-expensive. And the hyperbaric oxygen therapy treatment cost is not low, basically between $200 and $400 a time. Moreover, not every hospital has a hyperbaric oxygen chamber. If it is determined that HBOT treatment is needed for a long time, you can consider purchasing a hyperbaric oxygen chamber for home or renting a hyperbaric oxygen chamber.
- Not a substitute for conventional therapy: It is not a substitute for revascularization (if the patient has severe large vessel occlusion). If there is a lack of proper blood flow, the effect of oxygen alone will be greatly reduced.
Contraindications:
- Untreated pneumothorax: life-threatening in a high-pressure environment.
- Recent middle ear or sinus surgery: Risk of Middle Ear Barotrauma and Sinus Barotrauma.
- With severe COPD or emphysema: potential risk of barotrauma and air embolism.
Summary
In summary, the positioning of hyperbaric oxygen therapy in diabetic complications is very clear: it is an effective auxiliary means for the treatment of refractory diabetic foot ulcers. It corrects the local hypoxic environment through physical principles, thereby promoting healing and assisting in anti-infection.
But it cannot replace basic blood sugar control and systematic wound care. Multidisciplinary collaboration is the key to maximizing the effectiveness of HBOT.





No Comment! Be the first one.